
Man proposes, God disposes
Blog Space / Man proposes, God disposes

- The Motherhood Factor
- The “Higher" Connection
- Man proposes, God disposes
- From Pessimism To Optimism
- Finding 'Sanjivani', Daily! (Part-7)
- Finding 'Sanjivani', Daily! (Part-6)
- Finding 'Sanjivani', Daily! (Part-5)
- Finding 'Sanjivani', Daily! (Part-4)
- Finding 'Sanjivani', Daily! (Part-3)
- Interesting case of pneumonia
- Finding 'Sanjivani', Daily! (Part-2)
- On the moment of 100th Pulmonology Teleconsultation
- Finding 'Sanjivani', Daily
- Why so "Breathless"?
- A Blessing in Disguise
- The Art of Taking Consent
- The Oldman's Pursuit
He was young adolescent , confused and in search of definite answers. And yes, he was breathless, too. Accompanying his father showing all the reports and describing his (short) history : an 'episode' of pneumonia 3 months back (Only symptom : Right sided chest pain)- diagnosed on X-ray chest & treated with 2 weeks course of antibiotics elsewhere. Relatively asymptomatic for nearly 2 months & developing almost same X-ray pattern with new symptom : breathlessness - which was increasing - so much that, he hardly slept for past 7 days.
I studied the reports. He was given 'reasonably acceptable' care. His CT Thorax was done 15 days back, showing areas of consolidation in right upper lobe with large mediastinal lymphadenopathy along with sliver of pleural effusion on right side - a classic description of 'Tuberculosis' & hence he was started empirically on the treatment according to weight - which he was not tolerating.
In my opinion, there was 'gross' discrepancy between his clinical history & radiological findings. He didn't have cough, sputum, fever, anorexia or weight loss - making clinical likelihood of tuberculosis relatively less. The other important conditions which present like this were sarcoidosis - a multi system disorder, lymphoma - a type of cancer - common at this age - however absence of fever was going against it & a remote possibility of carcinoma - a neoplastic process - a long shot in view of no family / occupational / smoking history.
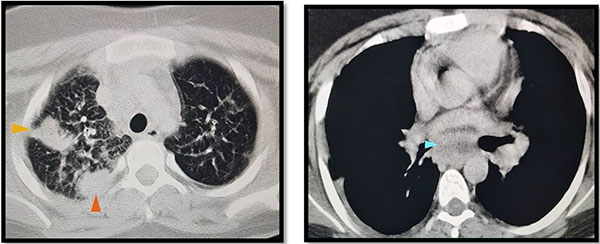
(Images of CT Thorax : on left : lung window showing consolidation areas in right upper lobe, on right : mediastinal lymphadenopathy – highlighted with arrows)
I admitted him in ward with agreement to shift him in ICU anytime if need arises - as he was breathing at the rate of 36 breaths per minute - almost twice the rate of normal individual at his age. His preliminary evaluation did not reveal any major organ damage nor any external site of tissue sampling or tappable pleural fluid - meaning that, I need to focus on a focus : which was lung & mediastinal lymphnodes. The discussion with radiologist concluded with inability to perform CT guided procedure at such high respiratory rate & a diagnostic tip : to prioritize mediastinal node over lung tissue.
The Thumb rule of medicine is : diagnostic investigative procedure should not result in deterioration from the existing health condition. I had only two options left with me:
To intubate him for the sake of Bronchoscopy & Esophageal Ultrasound guided sampling: which will give definitive answers but than elective intubation is inevitable
To wait for deterioration of his health status - which anyways will require intubation & may lead to losing the chance to give him final diagnosis
We did not have much time, as he was sitting on an edge with impending fatigue of respiratory muscles. I explained the dilemma, and finally we agreed to proceed for elective intubation & minimally invasive procedures.
The procedures went smooth. As expected he didn't give me much time in tracheobronchial tree owing to hypoxia - so that I could only inspect the airways & collect bronchial wash but the 'tip' worked & we fetched enough tissue from the large necrotic subcarinal lymphnode. Even than, we were having 'gut feeling' of tuberculosis. He was quite settled & according to our critical care experts, worth to be extubated the day after, giving us relief and high hopes of recovery.
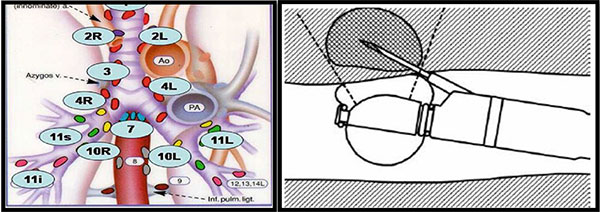
(In images: Schematic diagram of mediastinal lymphnodes on left, endoscopic ultrasound guided sampling of lymphnode on right)
However, destiny decided something else. By evening we started getting the reports one by one: No trace of tuberculosis, sarcoidosis or lymphoma and definite presence of poorly differentiated carcinoma cells with IHC markers positive for primary in lung. Final diagnosis : Primary adenocarcinoma of lung. In 24 hours of admission, he was diagnosed a terminal illness requiring palliative care. Medical oncologists came on board & started the evaluation towards same.
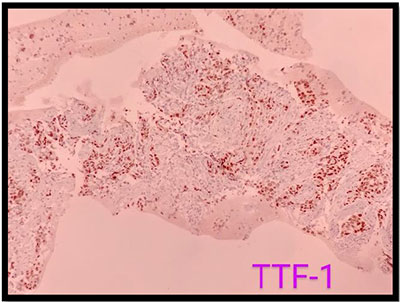
(In image above :TTF-1 Positive malignant cells)
We didn't break anything to him except the schedule of IPL matches & scores, however his father was well informed about overall prognosis. He accepted the fact & was prepared for the future battle. Deep-down, almost all of us involved in his care were happy after the tremendous accomplishment & successful fetching of a rare diagnosis and at the same time feeling sad because though theoretically the final diagnosis was plausible, it was quite difficult for us to digest. Indeed, we witnessed the literal meaning of saying "Man proposes, God disposes".
The incidence of primary lung cancer in persons under 18 years is less than 0.05/100,000 persons , and primary pulmonary adenocarcinoma constitutes <10% of all cases. The diagnosis of such rare condition requires dedication, discipline & team work. I acknowledge support from: Dr. Nilay Mehta & team (Dept. of Medical Gastroenterology), Dr. Tejash Parikh & team (Dept. of Critical Care Medicine), Dr. Sandeep Sheth , Dr. Loma Parikh & team (Dept. of Histopathology), Dr. Gaurav Goswami & team (Dept. of Radiodiagnostics), Dr. Pankaj Shahsir/Dr. Mithun Shah & team (Dept. of Medical Oncology) as well patient transfer team & endoscopy staff for active participation.
Dr. Jaykumar Mehta
MBBS (Gold Medalist)
MD, DNB, MNAMS, PD Fellow (Pulmonology)
Consultant Interventional Pulmonologist (Zydus Hospital, Ahmedabad)


