
Cardiology
Medical Specialities / Cardiology

FAQ
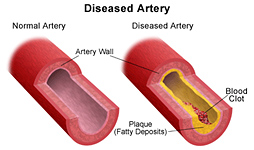
Coronary artery disease (CAD) occurs when the arteries supplying blood to the heart / cardiac muscles (coronary arteries) become hardened and/or narrowed. This occurs due to the buildup of plaque on the inner walls or lining of the arteries (atherosclerosis). Blood flow to the heart is reduced as plaque narrows the coronary arteries. This decreases the oxygen supply to the heart muscle.
Your arteries are normally smooth and unobstructed on the inside, but as you age, a substance called plaque can build up in the walls of your arteries. Plaque is made up of cholesterol, calcium, and fibrous tissue. As more plaque builds up, your arteries narrow and stiffen. This process is called atherosclerosis, or hardening of the arteries.
Coronary artery disease (CAD) is the most common type of heart disease. It is amongst the leading cause of death in both men and women. Lifestyle changes that may lower your risk are as follows:
- Stop smoking
- Control diabetes
- Control blood pressure
- Be physically active
- Eat a low-saturated-fat, low-cholesterol diet
When blood flow and oxygen supply to the heart are reduced or cut off, you can develop:
Chest pain (angina) or discomfort : This occurs when your heart is not getting enough blood. If your angina symptoms return or you experience symptoms such as pain, fullness, tightness or burning in your chest, arms, or neck, you need to let your physician know right away. It may mean that the blockage has reoccurred.
A heart attack occurs when a blood clot suddenly cuts off most or all blood supply to part of the heart. Cells in the heart muscle that do not receive enough oxygen-carrying blood begin to die. This can cause permanent damage to the heart muscle.
Over time, CAD can weaken your heart muscles and contribute to Heart/Cardiac failure. Heart failure does not mean that your heart has stopped or is about to stop working. But it does mean that your heart is failing to pump blood the way that it should.
Heart failure ca also be a resultant of Arrhythmias; which are changes in the normal rhythm /irregular heartbeats.
Or to arrhythmias; which are changes in the normal rhythm of the heartbeats – IRREGULAR HEART BEATS.
A Cardiac Angiography (CAG) is the best way to detect the extent of blockage and determine the further line of treatment.

Your treatment will depend on the severity of your condition, and whether or not you are having symptoms from the carotid artery disease, as well as your general health. As a first step, your physician may recommend medications and the lifestyle changes.
Medical Therapy : There are a number of medicines that can be used to improve symptoms of coronary artery disease and to prevent future heart attacks
Coronary Artery Angioplasty: is a non-surgical procedure that can be used to dilate (widen) narrowed or blocked arteries when symptoms are severe or when the blockage occurs in a dangerous location. A thin tube called a catheter with a deflated balloon on its tip is passed into the narrowed artery segment. After the balloon is inflated to widen the artery, the balloon is deflated and the catheter is withdrawn.
Stenting: It is a non-surgical procedure where a tiny metal coil is expanded inside the blocked artery to open the blocked area and is left in place to keep the artery open.
Atherectomy: It is a non-surgical procedure that inserts a tiny device on the end of a catheter inside the artery and the plaque is "shaved" away.
CABG: Coronary Artery Bypass Surgery (or open heart surgery) is a surgical procedure for patients with extensive blockages.
- ECG
- ECHO
- TMT
- Holter Monitor
ECG (Electrocardiogram/Electrocardiography) : An ECG gives a recording of the electrical activity of the heart. Electrodes are positioned on the chest, wrists and ankles and a recording is made. It reflects what is happening in different areas of the heart and may show up an abnormality or previous damage.
Echocardiogram : Also referred to as an 'echo' this is an ultrasound scan of the heart. Sound waves bounce information about the structure of the heart back to a computer to make a picture of the heart. This tells the doctor about:
- The size of the heart
- How well the muscle is working
- How well the valves are working
TMT (Treadmill test) : An exercise stress test that usually involves walking on a treadmill or riding a stationary bike while your heart rhythm, blood pressure and breathing are monitored. Your doctor may recommend an exercise stress test if he or she suspects you have coronary artery disease or an irregular heart rhythm.
Holter Monitor : A Holter monitor is a continuous tape recording of a patient's ECG for 24 hours. Since it can be worn during the patient's regular daily activities, it helps the physician correlate symptoms of dizziness, palpitations (a sensation of fast or irregular heart rhythm) or black outs. Since the recording covers 24 hours, on a continuous basis, Holter monitoring is much more likely to detect an abnormal heart rhythm when compared to the ECG which lasts less than a minute. It can also help evaluate the patient's ECG during episodes of chest pain, during which time there may be telltale changes to suggest ischemia or reduced blood supply to the muscle of the left ventricle.
The tilt-table test is helpful in identifying the causes of fainting. As suggested by its name, the tilt table test involves placing a patient on a table with a foot-support, table is then tilted upwards. The tilt-table starts off in a horizontal position and is tilted gradually by degrees to a completely vertical position. While the test is underway patient's blood pressure, pulse, and symptoms are continuously monitored throughout the test.
The tilt-table test is helpful in detecting the common causes of fainting or lightheadedness, this phenomenon is also known as postural hypotension (orthostatic hypotension). Tilt-table testing may be usually performed when a heart disease is not suspected to be the primary cause for being responsible to cause an attack of fainting (syncope).
- Coronary Angiography
- CT Angio
- Thallium Test
Coronary Angiography is the Gold Standard single test to diagnosis Coronary Artery Disease. It is very safe, effective, less time consuming and highly reliable. The procedure involves using a special dye (contrast) and x-rays to see how blood flows through the arteries in your heart. Often done along with cardiac catheterization, this is a procedure which measures pressures in the heart chambers.
Before the test starts, you will be given a mild sedative to help you relax and make the procedure pain free.
An area of your body (the arm or groin) is shaven (if needed), cleaned with an anti-bacterial solution and numbed with a local numbing medicine (local anesthetic). The intervention cardiologist passes a thin hollow tube, called as catheter, through an artery which is carefully moves up into the heart. Continuous X-ray images help the doctor position the catheter.
Once the catheter reaches the desired place, dye (contrast material) is injected into the catheter. Continuous X-ray images are taken to see how the dye flows through the arteries, the skillful and trained eyes of the cardiologist picks up the blockages (if any) and the patient is advised accordingly.
The procedure most often lasts 30 to 60 minutes.
The same procedure is used to determine blockages in other vessels like Renal artery (Kidney).
Angiography is the X-ray imaging of blood vessels using contrast agents injected into the bloodstream. CTCA uses computed tomography (CT) scanning to take pictures or images (angiograms) of the coronary arteries of the beating heart. These arteries supply blood to the heart muscle, and disease of these vessels (atherosclerosis) is responsible for most heart attacks. Liquid contrast agents, sometimes called contrast medium, are injected into a vein (usually in the arm). Contrast agents increase the density of the blood in the vessels, and allow the inside and outside structure of blood vessels to be clearly visible on the CT angiogram images.
Medication to reduce blood flow and slow down the heart rate might also be given to make the images even clearer and easier to interpret. This will either be given in tablet form or into a vein through a cannula (a thin plastic tube) inserted in the arm.
Coarctation of the Aorta is a congenital (birth) defect of the major cardiac artery (aorta) which carries the blood from the heart, to every other part of the body to supply oxygen and other nutrients. As an alternative to surgical repair, some people with coarctation of the aorta may be candidates for a cardiac catheterization procedure which involves passing a balloon and a device called a stent, into the area of the narrowing, which can be inflated to expand the narrowed area and keep it open.
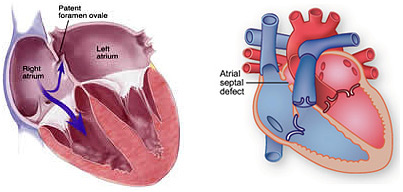
A PFO is similar to an atrial septal defect (ASD). It is a flap-like communication in the dividing wall, which allows abnormal flow between the upper two chambers of the heart. Unlike an atrial septal defect, every baby is born with this flap which is a critical part of the fetal circulation. In 80% of all people, the two pieces of the flap fuse completely together forming a solid wall after birth. A double umbrella device can be passed to the heart through a small tube introduced at the leg, just as with repair of the atrial septal defect.
Carotid artery disease occurs when the major arteries in your neck become narrowed or blocked. These arteries, called the carotid arteries, supply your brain with blood. Your carotid arteries extend from your aorta in your chest to the brain inside your skull.
Structural heart disease most often refers to cardiac defects which are congenital in nature (birth defects), but may also include abnormalities of the valves and vessels of the heart wall that develop with wear and tear on the heart, or through other disease processes. The three most common congenital heart diseases are Atrial Septal Defect (ASD), Patent Foramen Ovale (PFO), and Coarctation of the Aorta.
An ASD is a hole in the wall (septum) which separates the top two chambers of the heart. A PFO is similar to an ASD; it is a flap-like hole in the wall that separates the upper two chambers of the heart, a coarctation of the aorta is a narrowing of the vessel, in the upper chest that carries the blood from the heart, to every other part of the body to supply oxygen and other nutrients.
In PFOs :
- Transient Ischemic Attack (TIA or mini-stroke)
- Migraine headaches
- Low oxygen levels in rare patients
- “Bends” in divers
In ASDs :
- Heart palpitations
- Exercise intolerance
- Stroke
In Coarctation of the Aorta :
- High blood pressure in the arms and head w/ low or normal blood pressure in the legs
- Stroke
- Premature coronary artery disease (CAD)
- Leg cramping when exerted
- Kidney dysfunction
There are treatments in the catheterization lab for ASDs, PFOs and coarctations. For both ASDs and PFOs there is a catheter based procedure that utilizes specific closure devices. Stenting is used to treat patient’s coarctations.



