
A Blessing in Disguise
Blog Space / A Blessing in Disguise

- The Motherhood Factor
- The “Higher" Connection
- Man proposes, God disposes
- From Pessimism To Optimism
- Finding 'Sanjivani', Daily! (Part-7)
- Finding 'Sanjivani', Daily! (Part-6)
- Finding 'Sanjivani', Daily! (Part-5)
- Finding 'Sanjivani', Daily! (Part-4)
- Finding 'Sanjivani', Daily! (Part-3)
- Interesting case of pneumonia
- Finding 'Sanjivani', Daily! (Part-2)
- On the moment of 100th Pulmonology Teleconsultation
- Finding 'Sanjivani', Daily
- Why so "Breathless"?
- A Blessing in Disguise
- The Art of Taking Consent
- The Oldman's Pursuit
Sitting in front of me was a "Non-Smoker" gentleman in seventies, a patient in his otherwise ‘full health’, accompanied by his granddaughter. The reason for obtaining my opinion was referral of a family physician, as the patient was coughing up blood (known as ‘Haemoptysis’ in medical language) since at least 6 months with almost daily occurrence for last 15 days. There was no other symptom like fever, loss of appetite, weight loss neither the amount of blood coughing up was alarming. I reviewed the medications, which did not include any blood thinner. He did mention suffering with asthma - almost since he was in his thirties & was also using regular inhaler medications for same - which he increased on his own to control the symptom of breathlessness owing to setting in of monsoon- as he did every year.
They brought the CT scan report mentioning a "mass", size of just more than 4 centimeters in the lower lobe of right lung : Postero-Medial basal segments to be specific. They wanted to undergo bronchoscopy: a minimally invasive procedure in which, with the help of camera at the tip of a flexible tube, one can visualize the airways as well as perform the guided procedures which involve sampling with saline called Broncho-Alveolar Lavage and sampling a lung tissue with forceps called biopsy - which can diagnose the condition & guide definitive treatment.
On examination (obviously with physical distancing & adequate protection), I found wheezing all over his chest. Fearing the airway manipulation during bronchoscopy can exaggerate the state of inflammation & narrowing of his already inflamed airways, I advised admission for optimization of his asthma prior to the procedure. Also, I wanted to plan the procedure meticulously.
The logical reasoning was:
It was "Solitary Pulmonary Nodule (SPN)", meaning there was no other site from where we can sample & obtain the diagnosis.
If I can achieve the diagnosis (which most probably will be neoplastic), according to TNM staging, he will be in stage IIA, where a definitive procedure is possible to get rid of the tumor.
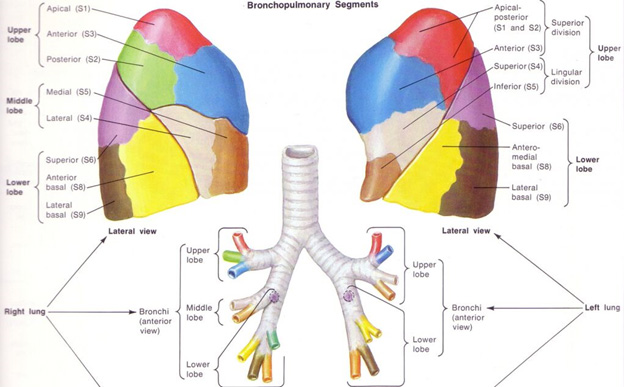
However, the procedure was not that easy. According to the basic anatomy, lungs are divided in to lobes by the fissures, which can be further subdivided into bronchopulmonary segments. Each bronchopulmonary segment is served by corresponding branches of the bronchial tree (airways), along with their own arterial supply. However, the venous and lymphatic vessels pass through the intervening septae that separate the segments from each other. The segments are separated from each other by bands of connective tissue. As a result, each bronchopulmonary segment is functionally separate from the adjacent segments.
Lungs are air filled spongy structures. Using needles or forceps can puncture it resulting in escape of air – causing a medical condition called pneumothorax. Usually this is minor, but still, a complication is a complication. I wanted to avoid it at all, as the patient was suffering from asthma and for that I had to be extra cautious.
The lesion was "airway centric" & hence any trans-thoracic approach will definitely lead to pneumothorax. On one hand, I wanted to prevent complications, while challenge on the other hand was to get the diagnostic yield. The studies have shown that, bronchoscopy gives excellent yield (more than 80%) when the lesion is bronchoscopically visible, the same will be less than 40%, if I will not be able to see it. According to the CT scan the lesion was in distal airway, meaning, 95% chances that I will not be able to visualize the lesion. I will be "on my own" in unknown territory, however as it was Type 1 lesion, according to the tumor-bronchus relationship types by Tsuboi et al, the bronchoscopy was the procedure of choice to sample it.
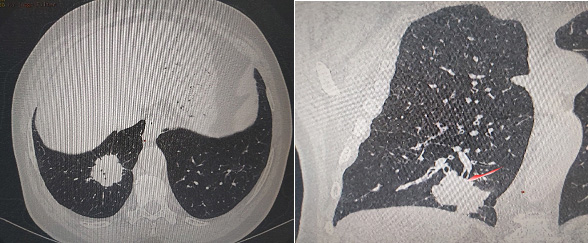
(In Images : CT Thorax plates showing location of mass lesion in right lower lobe with ‘bronchus cut off’ sign)
Keeping all these in mind, bronchoscopy guided biopsy was done and it was completely uneventful. As expected, the lesion was not visible but the skillfully executed biopsies from the medial basal segment of right lower lobe fetched enough tissue. The patient was discharged on the next day with optimized asthma medications & with the final diagnosis- to be followed up for curative intent.
According to World Health Organization (WHO) - cancers of the lung are among the top cancer types with approximately 2.1 million diagnosis worldwide in the year of 2018. It also amounts to the largest number of cancer related deaths. (1) From the various reasons responsible for this scenario, the most important one I believe is, failure to detect it ‘early'. However, as evident in the gentleman’s case, the frightening symptom of haemoptysis actually resulted in the early detection of a dangerous condition.
The carry home message is : Haemoptysis or coughing up blood is never normal. It is one of the “Red Flag” signs & has to be attended as early as possible. It can be a blessing in disguise if addressed wisely in time.
Dr. Jaykumar Mehta
MBBS (Gold Medalist)
MD, DNB, MNAMS, PD Fellow (Pulmonology)
Consultant Interventional Pulmonologist (Zydus Hospital, Ahmedabad)


