
Interesting case of pneumonia
Blog Space / Interesting case of pneumonia

- The Motherhood Factor
- The “Higher" Connection
- Man proposes, God disposes
- From Pessimism To Optimism
- Finding 'Sanjivani', Daily! (Part-7)
- Finding 'Sanjivani', Daily! (Part-6)
- Finding 'Sanjivani', Daily! (Part-5)
- Finding 'Sanjivani', Daily! (Part-4)
- Finding 'Sanjivani', Daily! (Part-3)
- Interesting case of pneumonia
- Finding 'Sanjivani', Daily! (Part-2)
- On the moment of 100th Pulmonology Teleconsultation
- Finding 'Sanjivani', Daily
- Why so "Breathless"?
- A Blessing in Disguise
- The Art of Taking Consent
- The Oldman's Pursuit
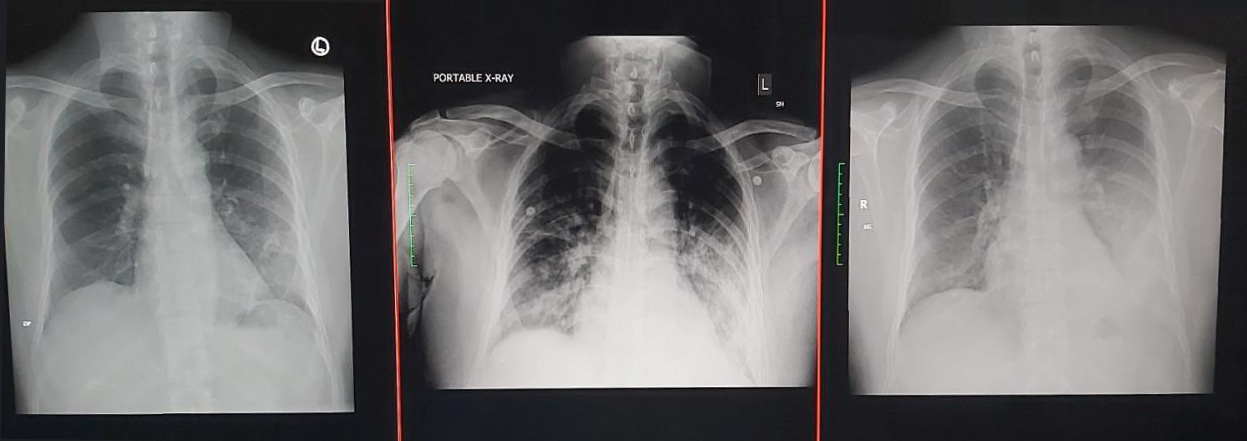
An immunocompetent hypertensive gentleman in fifties was shifted to Zydus Hospital, Ahmedabad for evaluation of Non-Covid pneumonia. The radiology was showing dense peripheral air space consolidation of left lower lobe with mild (Non-tappable) ipsilateral sympneumonic pleural effusion. His history was favoring acute onset illness with 7 days of duration & hospitalization elsewhere for one day to ascertain covid status.
His examination on the day of admission revealed SpO2 of 95% on room air & tubular type of bronchial breath sounds over left infra-scapular & infra-axillary region with no crepitations. He was started on empirical BL +BLI & macrolide antibiotics with supportive care.
His etiological evaluation revealed Klebsiella Pneumonie in respiratory panel. Although the antimicrobial coverage was good, clinically he was not responding - indicated by need of supplemental oxygen, presence of sputum purulence as well as development of fever spike (up to 99.6'F) after 48 hours of initial treatment. The antibiotic regimen was changed to Carbapenem, Fluoroquinolone & Linezolid suspecting drug resistant pathogen. He produced very little purulent sputum on that day, which was sent for culture & sensitivity.
His clinical condition remained status quo after 48 hours of upgraded regimen with no further fever spikes, but he developed new finding - crepitations over right infraclavicular & infrascapular region - a progression on right side confirmed with X-ray chest on same day. Anticipating further clinical deterioration, he was shifted to ICU - with culture confirming growth of GNB. He threw another fever spike on that day - indicating partial effect of regimen. After thorough discussion, acting patiently, we waited for drug sensitivity - which confirmed carbapenem resistance. The carba-R assay detected NDM & OXA-48 and the antibiotic regimen was tailored accordingly. After 48 hours of the regimen, the patient shown clinical-lab-radiological improvement after which he was shifted to ward & finally discharged with parenteral antibiotics.
His follow up after 14 days course of antibiotic regimen revealed near complete resolution in X-ray chest & normal breath sounds.
The most important aspect in the care of patient suffering from pneumonia is robust observation & close monitoring to suspect drug resistance at the earliest. Failing to detect it not only leads to progression of disease requiring intensive care with invasive or non-invasive ventilation but also to significant mental, social & financial disruption.
Community transmission of drug resistant pathogens is not commonly suspected, however we did witnessed koch's postulate in the gentleman's case. Due to timely & coordinated efforts - he was saved from prolonged hospitalization & advanced respiratory supports for which this pathogen is infamous.
(In Image: Serial X-rays in reverse order)
Dr. Jaykumar Mehta
MBBS (Gold Medalist)
MD, DNB, MNAMS, PD Fellow (Pulmonology)
Consultant Interventional Pulmonologist (Zydus Hospital, Ahmedabad)


