
From Pessimism To Optimism
Blog Space / From Pessimism To Optimism

- The Motherhood Factor
- The “Higher" Connection
- Man proposes, God disposes
- From Pessimism To Optimism
- Finding 'Sanjivani', Daily! (Part-7)
- Finding 'Sanjivani', Daily! (Part-6)
- Finding 'Sanjivani', Daily! (Part-5)
- Finding 'Sanjivani', Daily! (Part-4)
- Finding 'Sanjivani', Daily! (Part-3)
- Interesting case of pneumonia
- Finding 'Sanjivani', Daily! (Part-2)
- On the moment of 100th Pulmonology Teleconsultation
- Finding 'Sanjivani', Daily
- Why so "Breathless"?
- A Blessing in Disguise
- The Art of Taking Consent
- The Oldman's Pursuit
“ तीन हफ्तों से नली लेकर घूम रहे हैं साहिब, फर्क नहीं पड़ रहा है!” (Roaming around with the tube for three weeks without any improvement, Sir) said the gentleman in his thirties sitting in front of me carrying a tube inserted on right side of his chest, holding the drainage bag : a water filled bag connected to his chest tube. I could hear constant bubbling sound coming from the bag while he was speaking indicating that he has large hole in his lung tissue resulting in constant communication of air he breathes in routing out via bubbles.
He was farmer & a “good” smoker, who developed severe pain on the right side of his chest which woke him up on the beginning of the month of July 2020. Amongst the state of COVID fear, he managed to get the medical help & had him inserted a small chest tube in nearby health care facility. He got an education that the smoking might have caused it but in spite of 6 long days, he was still having bubbling with no healing. He was finally referred to higher centre, where he got his CT scan of thorax showing right sided thoracic cavity filled with air & presence of some amount of fluid which was compressing his right lung, while the chest tube was in position. He got only reassurance that, “one day, the lung will expand”. But, the destiny decided something else & finally he landed up at Zydus Hospital, Ahmedabad on fourth week of his illness.
He was having a condition called ‘hydropneumothorax’ with non-expansion of lung in spite of having chest drain in situ.
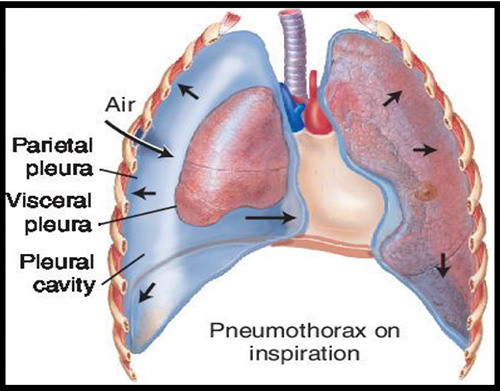
Before moving ahead, let me briefly narrate the physiology. Lungs are covered with membrane like structure called “Pleurae”. Each individual pleura is basically a twin layer: Outer layer (beneath the rib) called parietal pleura & inner layer (covering lung) called visceral pleura. There is thin film of fluid in the “pleural space” - the space between these two layers generating “negative pressure” mechanism, which leads to inflation of lungs when the rib cage expands during inspiration. In the gentleman’s case, the air & some abnormal fluid filled this space causing compression of underlying lung.
After his evaluation, I concluded that:
The chest tube is not draining air with the speed matching the one with which it is filling.
He will require corrective (and costly) surgery if the lung will not expand
Keeping this in mind, I wrote an X-ray Chest to determine the current condition.
And in no time, I got a call from Dr. Ajay Patelsir - our senior radiologist, alerting me for a possible tension pneumothorax on right side with possibility of lung herniation necessitating his admission. On digging dipper, I found that, he was inserted 16 Fr chest tube elsewhere which was very small in calibre to drain possible large leak from his lung. I inserted larger chest tube in the intercostal space just below the previous one. After satisfied with the working of it, I removed the old one.
The aim of any intervention is to restore physiology & hence to do so, I need to bring the negative pressure back so that lung apposes with rib cage & the hole is sealed. There was enough waiting & watching - being “ pessimistic”. So, I applied a small mobile dry seal chest drain which has in built valve to the newly inserted chest tube.
The medical reasoning is, though there is paucity of data showing advantage of valved mobile dry seal chest drain over the conventional ‘non-valved' ‘water-seal' chest drain, in view of ease of handling, dry seal has obvious advantages of avoiding repeated filling of water column as well as fear of spillage, leading to improved quality of life. On top of that, Valve allows to aspirate air without ‘re-entry', which can lead to faster lung expansion if its not trapped. More over, I had successful outcomes with that in many of my patients and hence the single centre experience was acceptable. (Mobile valved dry seal chest drain applied to chest tube in image below)

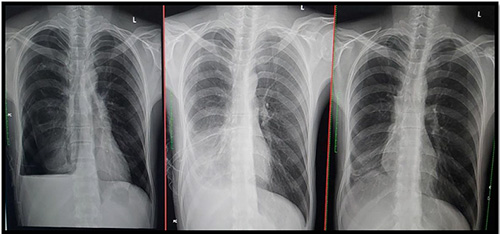
I drained approximately 2 Litres of air that day & explained the patient & his relative how to do it along with putting word of caution on maximum limit one can drain. Finally, he was happy that at least there was some active intervention. The reasoning helped and he drained almost 250ml of fluid on 3rd day. The fluid revealed heavy growth of pseudomonas – a virulent pathogenic bacteria. As his X-ray chest no longer shown signs of tension pneumothorax, he was discharged with drain in situ and with injectable antibiotics. On Day 10th of new chest tube & valved chest drain, his lower lung near completely expanded with a small air pocket in the upper part. Finally, on Day 20th, I clamped the tube for 24 hours and removed as there was no sign of air leak.
After receiving 51 injections to control the infection, his X-ray chest on beginning of September 2020 revealed near complete resolution of air & fluid level. I congratulated him on his patience & courage. His long quest finally came to end with the words, “जिंदगी के साथ कुछ अच्छा करूँगा, साहिब!”(Will do something good in life, Sir)
Lung healing in serial X-rays in the image below:
Dr. Jaykumar Mehta
MBBS (Gold Medalist)
MD, DNB, MNAMS, PD Fellow (Pulmonology)
Consultant Interventional Pulmonologist (Zydus Hospital, Ahmedabad)


