
ECMO
Medical Specialities / ECMO
FAQ
- ECMO is used to help people whose:
- Lungs cannot provide enough oxygen even when given extra oxygen through ventilator
- Lungs cannot get rid of carbon dioxide even with the help of ventilator
- Heart cannot pump enough blood to maintain all organs in the body
- ECMO may also be used to support people with heart or lung disease that cannot be cured while they wait for an organ transplant (e.g. new heart and/or lungs)
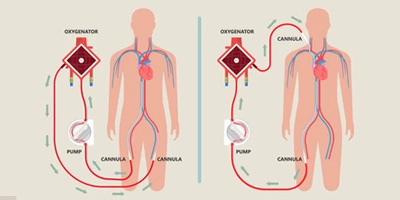
The ECMO machine is connected to a patient through plastic tubes (cannula). The tubes are placed in large veins and arteries in the legs, neck or chest. The procedure by which these tubes are placed in a patient is called cannulation.
The ECMO machine pumps blood from the patient's body to an artificial lung (oxygenator) that adds oxygen to it and removes carbon dioxide. Thus, it replaces the function of the person's own lungs. The ECMO machine then sends the blood back to the patient via a pump with the same force as the heart, replacing its function. The ECMO machine is controlled to give the patient the amount of heart and lung support they need.
Any patient connected to an ECMO machine in the ICU is also connected to monitors. These monitors measure heart rate, blood pressure, and oxygen levels. Patients on ECMO need their blood tested very often to measure the oxygen and carbon dioxide levels. These tests are called blood gases. Patients on ECMO are also given a medication to thin the blood so it does not clot. Thus, the blood is tested frequently to make sure it is thin enough.
An ECMO machine can help save a patient's life, but it does not treat the patient's disease or injury. An ECMO machine simply provides support for a patient while the medical team works on treating the underlying disease or injury (such as an infection) or until organs for transplant become available. Some diseases or injuries can be treated quickly, and patients only need the ECM() machine for a few hours. Other conditions may take longer to get better, in which case the patient may need the ECMO machine for several days to weeks. Unfortunately, in some cases, patients do not improve enough to be taken o the ECMO machine. ECMO does not save everyone but it has improved survival for many critically ill people who are not responding to usual life support options.
When a patient is being connected to an ECMO machine, he or she is sedated and does not feel the tubes going into their veins and arteries. A person on ECMO is usually already connected to a breathing machine (ventilator) through a tube (endotracheal or ET tube) that is placed in the mouth or nose and down into the wind-pipe.
Once connected to an ECMO machine, the cannulae are not painful. Patients who are on an ECMO machine may be given medicines (sedatives or pain controllers) to keep them comfortable. In some cases patients can be allowed to be awake and can talk and interact with people while on an ECMO machine. However, some movements can cause the ECMO tubes to get kinked, so patients need to be assisted and carefully supervised when they are awake.
The healthcare team looking after patients on ECMO aim to avoid any complications that may occur from being on the machine. Some of the more serious problems that may occur when a patient is on ECMO include:
Bleeding: Because of the blood thinning medication that patients need while on ECMO, they can start bleeding in different parts of their body. This can be a very serious problem if the bleeding happens in their brain, lungs, insertion sites of cannulae or from their stomach. The healthcare team monitors patients very carefully by frequent physical exams and lab tests to make sure there is no bleeding. If there is bleeding, then medications can be given to help the blood to clot. Blood and other blood products (such as platelets) may also need to be given if blood counts drop too low.
Kidney Failure: Patients who are on ECMO sometimes may due to various reasons do not get enough blood to their kidneys. If the kidneys stop working, then a patient may need to be connected to a machine that does the work of the kidneys. This is called dialysis. The kidney damage may get better.
Infection: The tubes from the ECMO machine go from outside the patient's body directly into their bloodstream. This increases the risk for infection, because the tubes are a way for germs to enter the body. The infection can reach the lungs, or any other part of the body. Infections in patients on ECMO can usually be treated with antibiotics. However, some patients who develop infections while on ECMO can get sicker and suffer organ damage.
Leg Damage: Some patients are connected to the ECMO ma- chine through a vein or artery in their thigh. In some cases, this can impair the blood flow down that leg, and the tissue in the leg can die. If this happens, doctors will try to get blood flowing back down the leg. This usually means changing the ECMO tubing to another part of the body. Unfortunately, the damage can occasionally be bad enough that the patient needs surgery to correct the problem, which may include amputation (removal of part of the leg).
Stroke:In patients on ECMO, certain areas of the brain may not get as much blood flow as they need because of small blood clots. This can cause a stroke, and parts of the brain may be permanently damaged. The area of the brain that is damaged will determine what problems a person has from a stroke.
The ECM() machine supports the patient while he or she tries to overcome a disease or injury. If the disease or injury improves, the patient may not need the support of the ECMO machine anymore. The healthcare providers will slowly reduce the amount of support the ECMO machine is providing to see if the patient will be okay without it, just like they do with a ventilator. If the patient remains stable (or improves) as this is being done, the ECMO tubes are removed and surgeons stitch the entry spots up to close them.
ECMO is only a "life-sustaining treatment." It does not cure or treat the disease or injury that led to heart and/or lung failure. This means it is a treatment that can prolong life to allow for more time to try to fix the problem. Sometimes patients may not get better despite long duration of ECMO support. A decision about whether there is benefit to continuing ECMO can be hard.
If the healthcare providers believe that the patient's disease or illness is very severe and will not get better, they will discuss this carefully with the family members and help to make decisions about the end of life care.



